Table of Contents
- Defining Policy and Procedure in Healthcare
- Why Clinical Policies and Procedures Matter
- Examples of Policies and Procedures in Healthcare
- Importance of Risk & Patient Safety Policies and Procedures
- What is PSWP?
- What is PSES?
- Benefits of PSO Membership
- Best Practices for Implementing Policies and Procedures in Healthcare
- The Future of Quality Care: Enhancing Patient Safety Through Policies and Procedures
In the ever-evolving landscape of healthcare, policies and procedures in healthcare are foundational to ensuring safe, efficient, and patient-centered service delivery. These frameworks not only address regulatory compliance but also enhance operational efficiency. With advancements in the field, the focus has shifted to the critical role of patient safety evaluation systems (PSES) and patient safety policies. This shift is driven by the need to create a culture of safety that fosters continuous improvement and transparent communication among healthcare professionals.
In this article, we delve into the intricacies of clinical policies and procedures, highlighting the integration of patient safety evaluation systems and their impact on enhancing the quality of care. By understanding these elements, healthcare organizations can better navigate the complexities of delivering top-notch care in an increasingly demanding environment.
Defining Policy and Procedure in Healthcare
The CDC defines policy as a “law, regulation, procedure, administrative action, incentive, or voluntary practice.” Policies often come from governing or oversight bodies but may also be implemented by individual healthcare organizations. For example, healthcare policies may address patient care, legal and safety regulations, or security and privacy matters.
In contrast, a healthcare procedure (not to be confused with a medical procedure) describes the steps undertaken to adhere to a policy. Think of procedures as the roadmap for showing how a policy should be implemented internally, describing the goals, actions, resources, and boundaries of the service. Both policies and procedures are data-backed and crafted by hospital administration and operations teams, with patient safety and quality of care as the top priorities.
Most crucially, neither healthcare policies nor procedures are static. Policies are often living documents, and procedures can and should be adjusted periodically to ensure adherence and compliance. These must be routinely reviewed and updated to evolve with clinical evidence, technology advancements, and more.
For example, The Joint Commission releases new National Patient Safety Goals each year based on qualitative and quantitative data from experts in the field. Organizations seeking accreditation frequently adjust their policies and procedures to adhere to current best practices as defined by these reputable organizations.
In addition to providing a structured framework and guidance on best practices, policies and procedures are essential to ensuring consistent standards of care and mitigating potential risks and adverse events.
Why Clinical Policies and Procedures Matter
The benefits of enacting strong, evidence-based policies and procedures in healthcare include:
- Standardization: Policies and procedures ensure consistency in treatment approaches, promoting equity among patient populations.
- Compliance: Policies and procedures ensure all team members follow legal and regulatory requirements and maintain high accreditation standards.
- Efficiency: Procedures help streamline workflows and processes, making care more timely and efficient. They reduce waste and redundancy without compromising on quality.
- Communication: Standardized policies and procedures make it easier for different practitioners and departments to communicate using a shared language. It is easier to collaborate and communicate when teams are working toward the same goals.
- Safety: Clear procedures place safety at the forefront, reducing medical errors and, thus, improving the quality of care.
For more insights on how to build an efficient and safety-focused environment, explore our high reliability organizations guide, which provides tools for creating and maintaining a high-reliability healthcare organization.
Examples of Policies and Procedures in Healthcare
Many policies and procedures in healthcare are essentially endemic in healthcare settings. For example, facilities have procedures in place to protect PHI according to HIPAA regulations. Likewise, hand hygiene policies and infection control procedures are put in place to protect both patients and staff from pathogens and infection.
Other examples of effective clinical policies and procedures include:
- Fall prevention policies and procedures;
- Patient Safety Evaluation System procedures;
- Discharge planning procedures;
- Medication administration procedures;
- Documentation standards for medical records;
- Policies for hazardous material management and disposal.
Importance of Risk & Patient Safety Policies and Procedures
The United States Congress showed its commitment to a culture of safety within our nation’s healthcare system in 2005 when it passed the Patient Safety and Quality Improvement Act. The Act, as it is commonly called, acknowledges that system failures are often best addressed when experiences, good and bad, are shared within an industry. The Act encourages open, honest discussion in a protected environment and promotes the development of a safer health system.
The protected environments referred to in The Act are Patient Safety Organizations or PSOs. As a byproduct of their daily work, healthcare organizations create a considerable amount of sensitive quality, safety, and risk-related information. Therefore, an organization’s participation in a PSO plays an important role in being able to use this information and conduct improvement activities in a protected space.
Part of the government’s rationale for establishing federal protections stemmed from the limited and inconsistent protections across states, which only fueled fear of legal liability and sanctions among physicians and healthcare organizations. So, unlike some state-specific protections that may only apply to certain circumstances or particular types of data, the PSO federal privilege and confidentiality protections apply to anything meeting the definition of Patient Safety Work Product or PSWP, including event details and associated deliberations.
For organizations looking to strengthen their patient safety strategies, joining a patient safety organization can be a pivotal step.
What is PSWP?
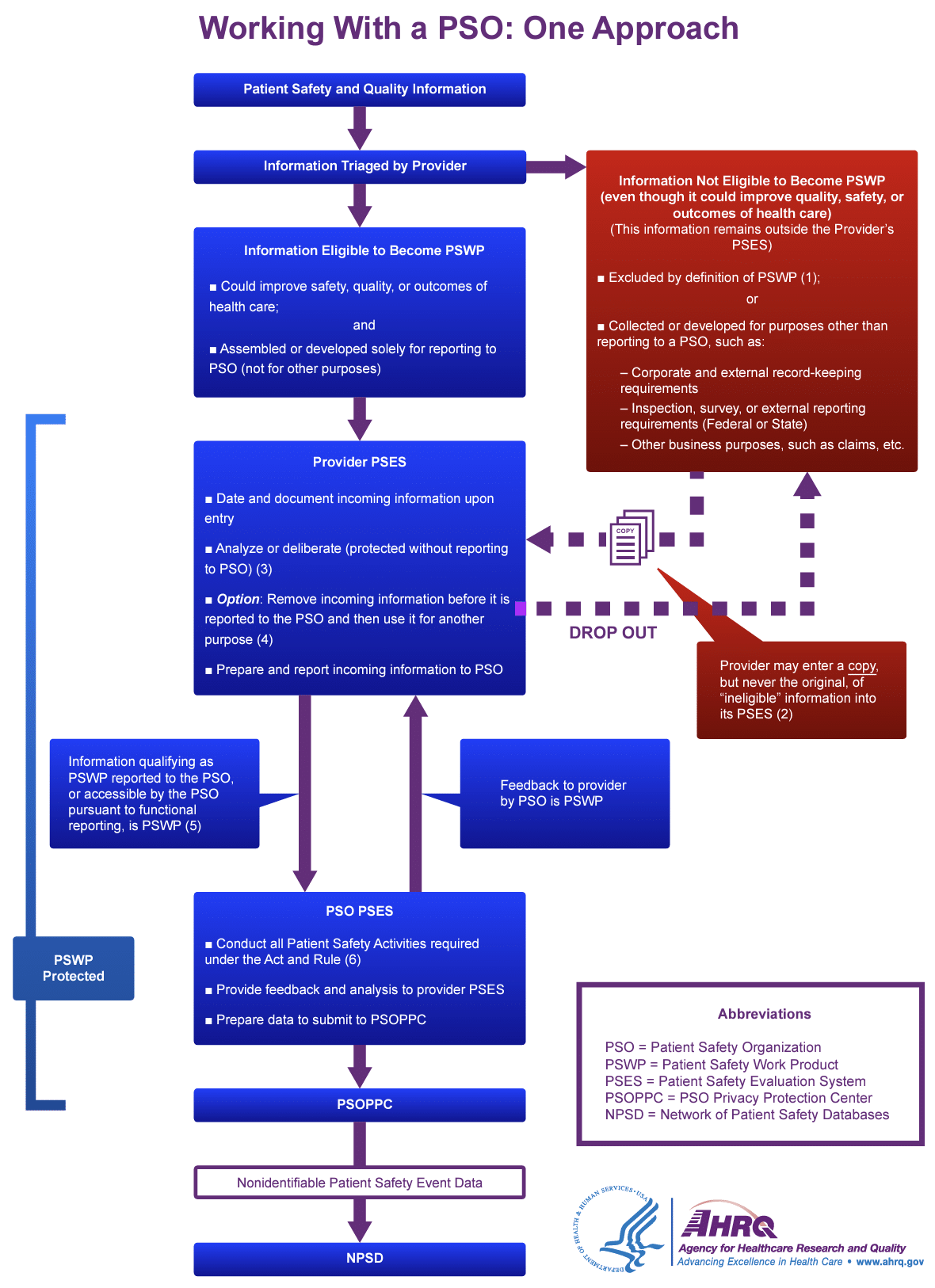
Patient Safety Work Product (PSWP) includes any data, reports, records, memoranda, analyses (such as root cause analyses) and written or oral statements (or copies of any of this material), which could improve patient safety, healthcare quality or healthcare outcomes, that are assembled or developed by a provider for reporting to a PSO and are reported to a PSO. PSWP also includes information developed by a PSO for the conduct of patient safety activities.
It’s just as important to define what PSWP is not. PSWP is NOT:
- Patient’s medical record
- Billing & discharge information
- Other original patient/provider information
- Other information collected, maintained, or developed separately or outside the Patient Safety Evaluation System (PSES)
- Other information collected & prepared for the purpose of meeting external obligations (e.g., state reporting requirements)
What is PSES?
A Patient Safety Evaluation System or PSES is the process that manages the collection, management, and analysis of information for reporting to a Patient Safety Organization (PSO). It’s characterized as the secure physical and/or electronic space for the conduct of patient safety activities. A PSES provides a protected environment for the candid consideration of quality and safety information. A facility’s PSES Policy is an important part of ensuring the full protection of PSWP under the law. While not required, it is considered best practice to document the mechanisms, staff, equipment, activities, and communication avenues your organization formally uses to manage PSWP.
In general, PSES policies should address the following:
- How information enters the PSES
- What processes, activities, physical spaces, and equipment are involved
- Which workforces need access to the PSWP in order to carry out duties
- What procedures or mechanisms the PSES uses to report information to a PSO or disseminate information outside the PSES
The PSES could include information from event reporting systems, root cause analyses, safety huddles, committee meetings/minutes, reports/dashboards/scorecards, and more. Given the importance of a PSES Policy in optimizing federal protections of privilege and confidentiality, patient safety organizations often assist members in designing and documenting the scope and function of their system.
For a practical resource, download our free Patient Safety Evaluation System Checklist.
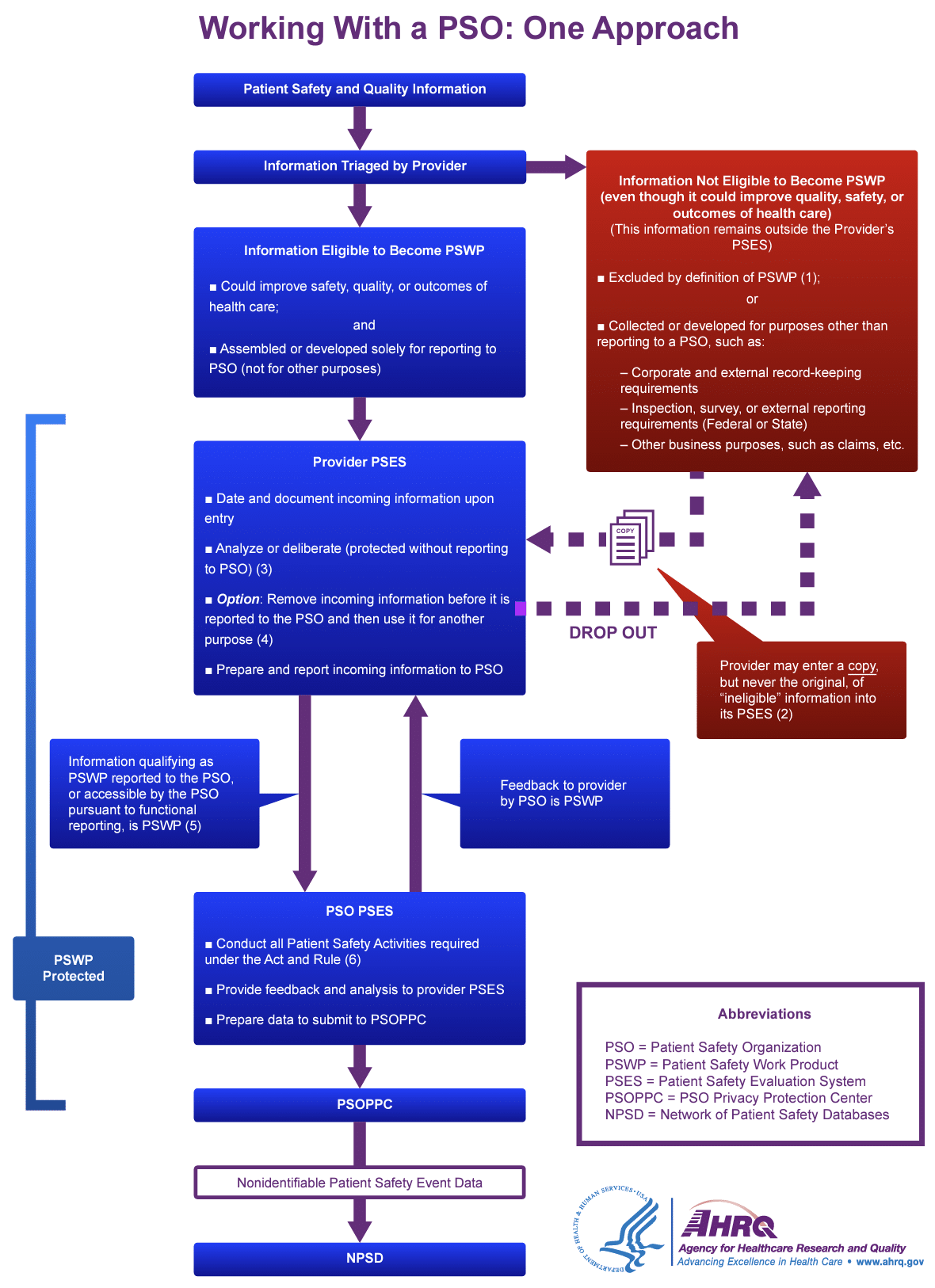
Source: AHRQ – Working with a PSO: One Approach
Benefits of PSO Membership
Becoming a Patient Safety Organization (PSO) was a natural extension of ADN’s commitment to enhancing policies and procedures in healthcare. In 2009, ADN was federally listed by the Agency for Healthcare Research & Quality (AHRQ). Following this, ADN launched its QAC event reporting application, a tool designed to collect and analyze event data. This application helps members identify underlying causes, redesign faulty processes, and ultimately reduce the risk and recurrence of safety errors.
The benefits of PSO membership, as outlined below, include federal protections and confidentiality, support with Patient Safety Evaluation Systems (PSES), detailed analyses, access to industry experts, and more.
Federal Protections & Confidentiality: Healthcare providers who report adverse events to a PSO are federally protected from legal discovery and can use the information to improve patient safety without fear of it being used against them in legal proceedings. This safe harbor encourages more reporting of adverse events, which can lead to a better understanding of the root causes of these events and help identify opportunities for improvement.
PSES Policy Support: ADNPSO provides its members with a comprehensive PSES Policy Template. Facilities are encouraged to integrate this template with existing policies and customize it to fit their specific workflows and processes, ensuring alignment with their policies and procedures in healthcare.
Analyses & Deep Dives: By collecting and analyzing data on adverse events, PSOs can identify patterns and trends that can help healthcare providers identify areas for improvement and implement strategies to reduce the incidence of adverse events. For example, in a deep-dive analysis by ADNPSO of all participant data, the event type “Other” revealed a death rate 3 times higher than ALL remaining patient safety event categories combined, demonstrating the value of detailed evaluation in refining healthcare policies and procedures.
Access to Experts & Initiatives: ADNPSO conducts patient safety activities with transmitted PSWP from our members to develop and disseminate best practices for improving quality and reducing adverse patient outcomes. Our most recent initiative focused on enhancing the safety culture within ambulatory care settings. This 18-month initiative not only benefited ADN’s clinic facilities but our acute care facilities as well. ADNPSO took the lessons learned from our work and developed resources applicable to the acute care setting. These resources were combined into a toolkit for PSO members.
Network of Patient Safety Databases (NPSD): The NPSD is a data source implemented by AHRQ that contains non-identifiable data derived from PSWP submitted to PSOs across the country. ADNPSO regularly contributes to the NPSD to support the learning of mitigating patient risk across healthcare settings, nationally. PSOs have the potential to promote rapid learning and widespread sharing of best practices, thereby enhancing policies and procedures in healthcare to improve patient safety.
Leveraging the Network: ADNPSO encourages members to proactively communicate with us about what they are focusing on, struggling with, or successfully improving. ADNPSO is always happy to share insights, as well as poll members or our AHRQ network. This dialogue can lead to productive email exchanges, virtual safe tables, or even larger PSO analyses or initiatives. For guidance on effective strategies, refer to our national patient safety goals guide.
Best Practices for Implementing Policies and Procedures in Healthcare
High-reliability organizations follow best practices for implementing policies and procedures in healthcare to ensure safety and quality care.
- Engage Relevant Stakeholders: Involve all key stakeholders, particularly frontline care staff, who have the most direct knowledge of what works and where improvements are needed. Their insights are invaluable when designing or revising policies and procedures, making the implementation process more effective and grounded in practical experience.
- Stay Current with Evidence-Based Updates: Ensure that policies and procedures in healthcare are continuously updated based on the latest clinical evidence. Tailor them specifically to your facility and patient population, using data sources such as patient safety data, near-miss data, and SOPS data.
- Prioritize Communication and Training: Effective communication is essential. Education and training for staff at all levels should be ongoing and comprehensive, ensuring that everyone understands the policies and procedures. The communication must be two-way, encouraging open dialogue between administration and care staff. This non-punitive approach promotes honest feedback, which is crucial for continuous improvement.
By fostering transparency and a data-driven mindset, acute care facilities can implement effective policies and procedures in healthcare that elevate the quality of care and enhance patient safety.
Join a Patient Safety Organization: Partnering with a patient safety organization can provide your facility with the resources, expertise, and legal protections needed to optimize your policies and procedures effectively.
The Future of Quality Care: Enhancing Patient Safety Through Policies and Procedures
The integration of comprehensive policies and procedures in healthcare with Patient Safety Evaluation Systems (PSES) marks a significant advancement in the pursuit of quality care. These frameworks not only ensure compliance with regulatory standards but also foster an environment of continuous improvement and patient safety. By adopting evidence-based practices and encouraging open communication through Patient Safety Organizations (PSOs), healthcare providers can significantly reduce medical errors and enhance patient outcomes.
Proactively engaging frontline staff, coupled with data-driven analysis and PSO support, builds a resilient healthcare system capable of adapting to new and emerging challenges. As the healthcare landscape evolves, the ongoing commitment to refining these healthcare policies and procedures will remain vital for achieving excellence in patient care.