Patient Handoff Templates: An Executive Guide to Safer Transitions
Poor patient handoffs are a silent risk to healthcare quality, often leading to preventable errors, prolonged stays, and costly consequences. This guide for executives dives into proven handoff strategies like I-PASS and SBAR, showing how hospital leaders can streamline transitions of care and improve outcomes. Learn how ADN’s patient safety event reporting application can help track handoff-related issues and drive meaningful improvements across your organization.
⏰ 12 min read
Table of Contents
Hospital executives nationwide are continually searching for ways to enhance quality improvement in healthcare. One key area often overlooked—but crucial to mitigating patient handoff errors—is the standardized patient handoff process. By refining patient handoff communication, healthcare leaders can strengthen patient safety, support staff efficiency, and improve overall organizational performance.
What Is a Patient Handoff and Why It Matters to Executives
Patient handoffs in patient care—sometimes referred to as “handovers”—involve transferring key information about a patient’s medical status, ongoing treatments, and relevant clinical details from one healthcare provider or team to another. These transitions occur frequently:
- Shift changes between nursing or physician teams
- Inter-departmental moves (e.g., from ICU to step-down units)
- Inter-facility transfers (e.g., from a rural hospital to a tertiary care center)
Key Stat: The Joint Commission estimates that miscommunication during care transitions is a leading contributor to patient safety events—including preventable harm and higher readmission rates. “Joint Commission data indicate inadequate handovers are a factor in 80% of all adverse events, which include wrong-site, wrong-procedure, or wrong-patient surgeries; treatment delays; medication errors; and falls,” according to a 2018 study on communication’s effect on patient safety.
For hospital directors and VPs, these errors directly impact metrics such as patient satisfaction (HCAHPS scores), value-based reimbursement, and accreditation readiness.
How Patient Handoff Errors Affect Hospitals
When a patient handoff fails—due to incomplete, untimely, or misinterpreted information—the potential harm ranges from minor complications to serious sentinel events. This risk multiplies with the high frequency of handoffs in patient care.
- Financial Impact: Medical errors and extended lengths of stay can lead to increased costs and reduced reimbursements.
- Accreditation and Legal Risks: Agencies like The Joint Commission may cite communication lapses in accreditation reviews, and litigation risks rise when errors occur.
- Reputation and Patient Satisfaction: Communication failures undermine patient trust and often negatively influence HCAHPS scores.
“Patient handoffs involve a structured communication process where the receiving caregiver ideally has the opportunity to ask questions and clarify details to fully understand the patient’s condition,” said Elizabeth Mort, MD, vice president and chief medical officer at The Joint Commission. “Healthcare professionals are deeply committed and work to ensure that patients’ needs are met, and optimal care is delivered. Regrettably, some of the important clinical detail can be lost during the transfer or transition of a patient to another healthcare provider for ongoing care.”
The Joint Commission suggests hospitals choose the patient handoff template that best fits their environment, but it emphasizes staff training, complete documentation, and cultural competency to prevent handoff communication breakdowns.
I-PASS vs. SBAR: Selecting a Patient Handoff Template
I-PASS: A Comprehensive, Evidence-Based Framework
I-PASS is a validated patient handoff tool designed to reduce medical errors and improve communication across multiple points of care. It was developed through a multi-institutional collaboration that sought to unify best practices from leading academic medical centers.
The acronym I-PASS stands for:
- Illness Severity:
Providers categorize the patient’s current status (e.g., stable, unstable, or requiring close monitoring) to quickly convey the level of urgency. - Patient Summary:
A concise overview of the patient’s chief complaint, diagnosis, and brief hospital course. This may include relevant medical history and any major interventions already performed. - Action List:
Specific tasks to be completed by the incoming caregiver—such as ordering tests, following up on lab results, or administering medications. Clear accountability prevents important to-dos from being overlooked. - Situation Awareness/Contingency Planning:
Potential issues to watch out for and predefined plans to address them (e.g., “If the patient spikes a fever, initiate a sepsis workup”). Proactively sharing “what-ifs” helps avoid delays when complications arise. - Synthesis by Receiver:
The handoff recipient paraphrases the information and clarifies any uncertainties. This “teach-back” step ensures mutual understanding and encourages collaborative problem-solving.
Why It Works:
- Evidence-Based: Multiple peer-reviewed studies show that adopting I-PASS can significantly reduce preventable errors, particularly in high-turnover environments like teaching hospitals.
- Structured and Specific: Each element of I-PASS addresses a unique piece of critical information, preventing important details from slipping through the cracks.
- Interdisciplinary: It’s adaptable for various roles—physicians, nurses, and allied health professionals—allowing everyone to speak a common “language” during handoffs.
SBAR: A Streamlined, Universal Approach
Originally adapted from the U.S. Navy’s communication protocols, SBAR (Situation, Background, Assessment, Recommendation) is another widely recognized framework for patient handoff communication. Its simplicity has made it a go-to method in many hospitals worldwide.
The acronym SBAR stands for:
- Situation:
A succinct statement of the patient’s current condition or the immediate problem (e.g., “Mr. Smith’s oxygen saturation is dropping”). - Background:
Relevant medical history, recent interventions, or any contextual information that might influence treatment decisions (e.g., “He has a history of COPD and was admitted for pneumonia”). - Assessment:
The outgoing caregiver’s clinical interpretation—what they believe is happening based on vitals, labs, and observed symptoms (e.g., “I suspect his infection may be worsening due to increasing respiratory distress”). - Recommendation:
Proposed next steps or desired actions from the receiving team (e.g., “We should obtain an arterial blood gas and consider IV antibiotics immediately”).
Why It Works:
- Concise and Flexible: SBAR’s four-step format is quick to learn and easy to remember, which is vital in urgent or fast-paced situations.
- Improves Accuracy: By requiring an explicit “Assessment” and “Recommendation,” SBAR encourages providers to form and share a clinical impression rather than simply relay data.
- Adaptable Across Departments: From emergency departments to perioperative settings, SBAR can be integrated into almost any workflow to facilitate clear communication.
Choosing Between I-PASS and SBAR
Both I-PASS and SBAR promote standardized patient handoff practices, reduce errors, and improve team collaboration. However, certain hospital environments may favor one approach over the other:
- I-PASS is often preferred in academic or teaching hospitals where detailed action lists and contingency plans are critical. Its structured “Synthesis by Receiver” step can be especially beneficial in multidisciplinary teaching rounds or complex inpatient settings.
- SBAR is widely adopted in fast-paced clinical areas—like the ER or ICU—because its four-step design quickly orients the receiver to the most urgent and relevant facts. It is also highly effective for nurse-to-physician communication when immediate clinical decisions are required.
Integrating I-PASS or SBAR Into Your Organization
- Policy and Procedure Development
– Write clear policies outlining which model to use (I-PASS or SBAR), in which situations, and who’s responsible.
– Provide patient handoff examples during training sessions to illustrate correct usage. - EHR Integration
– Customize existing EHR templates to include fields for I-PASS or SBAR.
– Ensure that patient handoff checklists are easy to locate and fill out, reducing the likelihood of missing key data. - Ongoing Training and Auditing
– Offer competency-based workshops and simulations for clinical staff.
– Conduct regular audits to confirm thorough handoffs and gather feedback for continuous improvement. - Measure Impact on Patient Safety and Outcomes
– Track patient handoff errors and near-misses in your patient safety event reporting application before and after implementation.
– Monitor patient satisfaction, staff satisfaction, and any relevant outcome metrics (e.g., falls, medication errors, readmission rates).
Handoffs and Event Reporting: Capturing Near Misses, Incidents, and Driving Process Improvement
Fostering a Just Culture Through Reporting:
Voluntary reporting is a primary method of event detection, which means frontline staff are the main source of information, making it possible to learn about fractured or flawed processes. They provide a unique perspective into everyday workflows that help uncover issues that may otherwise go unnoticed. Furthermore, an organization’s willingness to use these reports to learn from errors and implement changes that prevent future risk and harm are at the heart of a strong safety culture.
Encouraging staff to report near misses and incidents related to handoffs in your event reporting application creates an environment where reporting errors is viewed as an opportunity for learning rather than blame. This approach supports a patient safety culture by:
- Encouraging Transparent Reporting: When staff are assured that handoff-related issues can be reported without punitive repercussions, they are more likely to share near misses and actual errors.
- Empowering Frontline Staff: A culture that values open communication and learning helps team members feel more engaged and responsible for patient safety.
- Building Trust: Transparent handling of handoff events reinforces trust among clinicians, ultimately leading to more accurate and complete communication during transitions of care.
Capturing Handoff Near Misses and Failures:
Patient handoffs are a critical point in transitions of care where communication gaps can lead to errors. When these lapses occur—even as near misses or “good catches”—they provide invaluable data for improving patient safety. By integrating a standardized handoff template into your clinical workflow, hospitals can:
- Document Critical Details: Capture the who, what, when, where, and why immediately following an event through a structured Summary of Initial Report (SIR) in your event reporting application.
- Identify Trends: Utilize data from near misses and failures to recognize recurring issues, such as incomplete or untimely communication. If your event reporting application has dashboards that can be easily filtered, this is much easier.
- Facilitate Immediate Action: Trigger rapid response protocols by flagging high-risk handoff events, ensuring that remedial measures are enacted without delay.
Using Event Data to Drive Handoff Process Improvement:
Event reporting systems should be much more than repositories for data. They are powerful tools for continuous quality improvement. By systematically analyzing reported events related to handoffs, healthcare leaders can:
- Benchmark Performance: Compare incident rates before and after the implementation of a standardized handoff template (such as I-PASS or SBAR).
- Refine Protocols: Use actionable insights from event data to optimize handoff processes, ensuring that every communication contains all critical patient details.
- Close the Loop: Implement feedback mechanisms where frontline staff are informed about changes made in response to their reports, thereby fostering a cycle of continuous improvement and increased engagement.
Integrating these practices ultimately drives better patient outcomes by reducing preventable errors and enhancing overall care coordination.
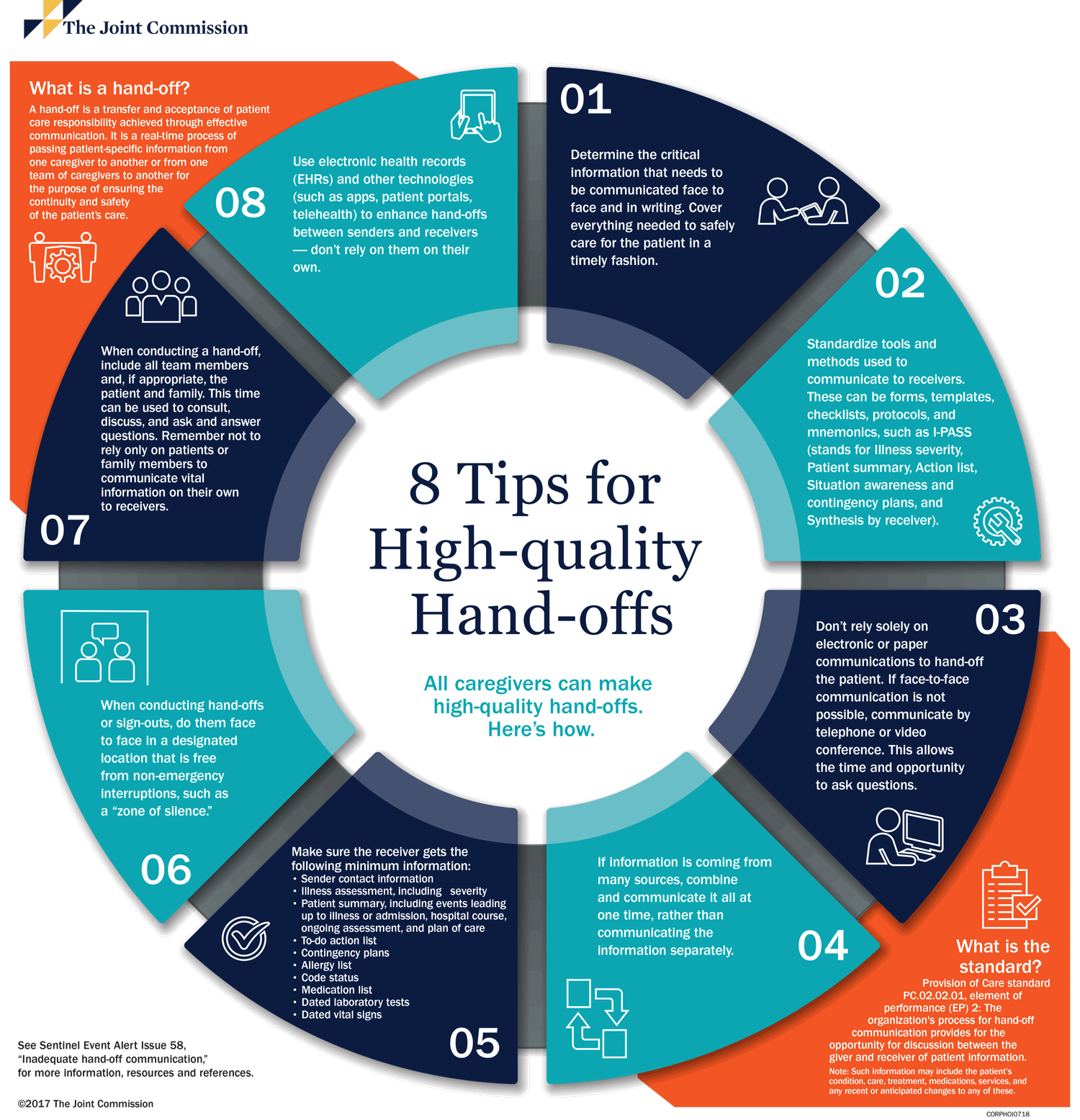
Patient Handoff Examples: 8 Tips for High Quality Handoffs
The Joint Commission created an infographic to help facilities implement better handoff practices. Download the patient handoff example infographic here.
The Role of Communication Bias in Patient Handoff Examples
Studies in JAMA Network Open and JAMA Pediatrics show how language bias during handoffs can lead to decreased empathy and even inaccurate recall of vital clinical details. When shifts in perception or hidden biases accumulate, patient care quality suffers.
In December 2024, a study published in JAMA Network Open revealed that when clinicians hear others describe a patient using negatively biased language—such as scorn, skepticism, or stereotyped-based assumptions—they have less empathy toward that individual.
Sometimes clinicians even become less accurate in recalling the person’s critical health details, including lab results, symptoms to pay attention to overnight, or recommended treatments. While such shifts in perception may be subtle and unintentional in many cases, as these hidden biases accumulate, they can influence the care that patients ultimately receive, the study’s authors pointed out.
“Biased language comes from our own implicit biases but can also affect others who do not necessarily hold the same biases,” said lead author Austin Wesevich, MD, MPH, MS, a hematologist and health services researcher at the University of Chicago Medicine. “When talking about a patient behind closed doors, it is important that doctors consider the impact the words they choose may have on other clinicians.”
Executive Perspective: Training staff to use neutral, fact-based language during handoffs and patient safety efforts can lower the risk of discrimination and improve care consistency—both of which align with accreditation standards and community trust.
Executive-Level Strategies for Success
- Align With Organizational Goals
– Highlight ROI: Show how improved patient handoff communication reduces falls, lowers liability, and raises patient satisfaction (HCAHPS).
– Set Clear Metrics: Define how many communication-related safety events or falls occur before and after implementing new protocols. - Adopt a Standardized Patient Handoff Tool
– I-PASS or SBAR Patient Handoff Example: Select a model that fits your facility’s culture.
– Integrate With EHR: Ensure that patient handoff templates are built into existing clinical workflows to minimize fragmented documentation. - Ongoing Education and Skill-Building
– Regular Training: Offer simulated patient handoff examples, focusing on real-world scenarios like early-morning falls.
– Peer Feedback: Encourage nurses, physicians, and ancillary staff to constructively critique one another’s handoffs. - Continuous Auditing and Improvement
– Establish KPIs: Track near-misses, sentinel events, and staff-reported handoff issues to measure progress.
– Conduct Random Spot-Checks: Validate the completeness of the patient handoff checklist.
– Adjust Rapidly: Use small tests of change (e.g., PDSA cycles) to refine handoff protocols. - Foster a Bias-Aware Environment
– Implicit Bias Training: Emphasize neutral, patient-focused language.
– Create a Safe Reporting Culture: Staff must feel comfortable reporting handoff gaps—like failing to note fall risks—without fear of punitive action.
Conclusion: Elevating Patient Safety and Reducing Costly Errors
For hospital directors and VPs, optimizing patient handoff communication is a strategic imperative. Standardized handoffs minimize patient handoff errors, enhance staff efficiency, and reduce preventable events—including serious patient falls at shift change. By adopting a structured approach, providing robust training, monitoring performance, and addressing bias, healthcare leaders can create a safer, more equitable environment that raises patient satisfaction and lowers organizational risk.
Next Steps
- Assess your current handoff protocols for gaps during shift changes.
- Implement a standardized model (e.g., I-PASS or SBAR), with emphasis on fall-risk communication.
- Track improvements in fall rates, safety incidents, and patient satisfaction over the next 6–12 months.
- Refine the process using feedback loops, technology integration, and ongoing education.
By prioritizing structured, consistent patient handoffs, hospitals can protect both patient safety and the bottom line—demonstrating tangible leadership in quality care.

